What are IBDs?
IBD (Inflammatory Bowel Disease: Crohn's disease and ulcerative colitis) are conditions characterized by severe intestinal inflammation that affect about 1.5% of the population in America and Europe, with direct and indirect management costs that have a significant impact on healthcare systems. Both the incidence and prevalence of IBD increase every year worldwide, especially in industrialized regions.
The etiology of this inflammation is still unknown, however several studies support the hypothesis that their onset is due to a combination and interaction of genetic, immune, and environmental factors. In particular, the latter seem to be fundamental in triggering the disease.
How does diet influence IBD?
Several studies have shown that certain nutrients exacerbate inflammatory bowel disease: a high intake of omega-6 polyunsaturated fatty acids (typical of the Western diet) as well as excessive consumption of animal proteins, particularly red meat, significantly worsen the active state of IBD. Their excessive consumption has direct effects such as the fermentation of animal proteins into ammonia, which weakens tight junctions, and indirect effects, by modulating the composition of the microbiota, making it poor in eubiotic and mucus-producing species such as Akkermansia muciniphila. Some dietary regimens are highlighted in several studies as solutions to reduce IBD manifestations, for example the low-FODMAP diet, the gluten-free diet, and the Mediterranean diet are associated with a reduction in disease flare-ups. These solutions, which must be implemented under the supervision of a Nutritionist, have always led to a modification of the gut microbiota with a development of eubiotic bacteria such as bifidobacteria and lactobacilli and butyrate-producing bacteria such as Faecalibacterium prausnitzii, with a simultaneous reduction of potential pathogens. Understanding how to modulate the gut microbiota through nutritional approaches could represent a strategy to control IBD, together with the use of probiotic bacterial species.
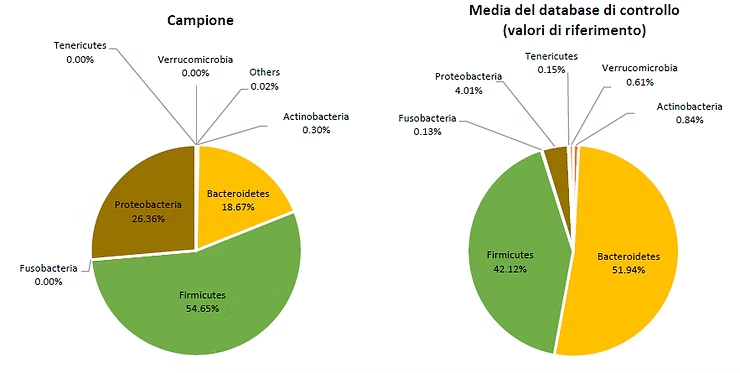
How are IBDs influenced by the microbiota?
In chronic inflammatory bowel diseases, genetic factors are not the only ones playing a key role in the onset of the disease. Several studies have shown that subjects with IBD are genetically more predisposed to having increased intestinal permeability: in these patients, anomalies are observed in the microbiota-host interaction, with the barrier effect being lost. Studies show that IBDs are clearly associated with significant intestinal dysbiosis, characterized by a reduction in biodiversity and a collapse of eubiotic species, butyrate producers, and bacteria that increase intestinal mucus production. The increase in intestinal permeability, associated with an increase in potentially pathogenic bacteria such as Escherichia coli and Fusobacterium nucleatum, further aggravates intestinal inflammation. This situation of intestinal dysbiosis also contributes to disease flare-ups.