Update: Mar 4, 2023
Endometriosis is a multifactorial pelvic disease associated with the accumulation of endometrial tissue outside its normal location (ectopic tissue). Cytokines, estrogens, stem and progenitor cells, and gut bacteria all have an effect on the development of endometriosis. Estrogens appear to play an important role: in a 2017 study, it was shown that estrogens were necessary to trigger endometriosis. In addition, they stimulate the growth and activity of ectopic endometrial tissue and inflammation. As with normal endometrium, ectopic tissue also reacts to hormonal fluctuations during the cycle, causing severe pain during menstruation, heavy menstrual flow, and pain during intercourse (dyspareunia).
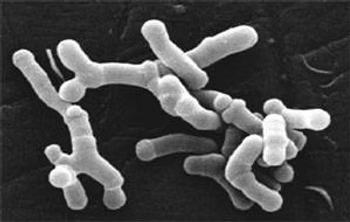
Gut bacteria influence estrogen metabolism through the action of the enzyme ß-glucuronidase, which is responsible for its conversion into the active form of estrogen that binds to estrogen receptors. The active estrogen then migrates to mucosal sites and ectopic tissue, causing the symptoms of endometriosis. Patients with endometriosis have more ß-glucuronidase-producing bacteria and a poor Firmicutes/Bacteroidetes ratio, resulting in putrefactive dysbiosis. If the microbiota is unbalanced, this can also affect the metabolites that stimulate the release of gonadotropin-releasing hormone (GnRH) in the brain. GnRH stimulates the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Both hormones lead to the production of estrogens and progesterone and increase estrogen secretion. This means that dysbiosis can trigger or worsen endometriosis. It has also been shown that microbial biodiversity is lower in patients with endometriosis. Biodiversity describes the variety of bacteria present in the gut: the more varied the bacterial composition, the more functions they can perform and the more resilient the microbiome is. Therefore, it plays an important role in the context of health. However, estrogens also have an influence on the microbiota, reducing its biodiversity.
Intervening on the gut microbiota in a highly personalized manner is therefore extremely important in the management of endometriosis and in addressing the specific dysbiosis of the person suffering from it, thus offering highly personalized and quality advice.