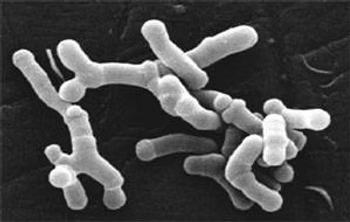
The human gut microbiome constitutes a diverse and dynamic community of microorganisms that populate the digestive tract. In recent years, a growing number of studies have explored the role of the gut microbiome in health and disease. Gut bacteria are involved in the pathogenesis of numerous medical conditions in a variety of medical fields including gastroenterology, metabolism, rheumatology, neurology, and psychiatry. Recently, evidence has emerged of the involvement of gut bacteria in chronic pain and particularly in fibromyalgia (FM). The composition of the gut bacterial community is altered in individuals with FM, with an altered abundance of a small subset of bacteria. The metabolic activity of these bacteria could be relevant in the expression of FM symptoms. The presumed mechanisms underlying the ability of bacteria to influence pain, fatigue, mood, and other symptoms include short-chain fatty acids, bile acids, neurotransmitters, and bacterial antigens. Understanding the role of the gut microbiome in chronic pain and particularly FM allows us to envision new and exciting future prospects for a better understanding, for the development of diagnostics, and for new therapies.
The gut microbiota in FM
The test uses the 16S rRNA sequencing technique (in Italy you can use the MyMicrobiota test, www.mymicrobiota.it). The general composition of the gut microbiome of patients with FM shows significant differences in the relative abundance of some short-chain fatty acid (SCFA) producing bacteria: Faecalibacterium prausnitzii and Bacteroides uniformis were found to be reduced in FM patients, while a greater abundance was observed for Intestinimonas butyriciproducens, Flavonifractor plautii, Butyricoccus desmolans, Eisenbergiella tayi, and Eisenbergiella massiensis. Species with a presumed pro-inflammatory role such as Prevotella copri, Bacteroides Uniformis, and Haemophilus parainfluenza were absent in FM patients, in contrast to their increase in inflammatory arthritis. Several members of the Bacteroides and Clostridium genera, both known for their established role in bile acid metabolism, were found to be differentially abundant in FM. Among these, Clostridium scindes, which is found in greater abundance in FM patients, is one of the few species that converts primary and secondary bile acids. Secondary bile acids derived from the microbiome are thought to sensitize nociceptors (pain receptors) by direct activation of endogenous bile acid receptors. Although the gut microbiome is generally correlated with multiple parameters including demographics, anthropometry, comorbidities, and drug characteristics, specific alterations of the microbiome in FM were found to be independent of the effect of these variations. Furthermore, the abundance of some species differentially abundant in FM was correlated with symptom severity.
Alterations in the gut microbiome of individuals with FM are not limited to the composition of the bacterial community, but involve significant changes in microbial metabolic function, with higher levels of butyric acid, lower levels of propionic acid, and similar levels of lactic acid observed in FM patients.
What you can do if you have fibromyalgia
- Stop taking random supplements and rely on a professional.
- Try to objectively assess how much FM symptoms impact your quality of life.
- Reduce stress.
- Use warm baths in the evening to relax your muscles.
- Purchase the "Adult Fecal Test" kit from MyMicrobiota (www.mymicrobiota.it) to assess your microbiota based on the most up-to-date scientific information. Together we can act to rebalance your personal dysbiosis, laying the foundation for your healing journey.